Ahinkorah, B. O. et al. Socio-economic and demographic factors associated with fertility preferences among women of reproductive age in ghana: Evidence from the 2014 demographic and health survey. Reproduct. Health. 18 (1), 2 (2021).
Odusina, E. K. et al. Fertility preferences among couples in nigeria: A cross sectional study. Reproduct. Health. 17 (1), 92 (2020).
Duminy, J. et al. Urban family planning in Low- and Middle-Income countries: A critical scoping review. Front. Glob. Womens Health. 2, 749636 (2021).
Hellwig, F. et al. Policies for expanding family planning coverage: Lessons from five successful countries. Front. Public. Health. 12, 1339725 (2024).
Khan, M. N. et al. Improving the uptake of contraception. Somalia Bull. World Health Organ. 102 (1), 75 (2023).
Mahasneh, I. & Ebrahim, F. The epidemiological declining in the human fertility rate in the Arab world for 10 years period 2011–2021. Middle East. Fertil. Soc. J. 29 (1), 47 (2024).
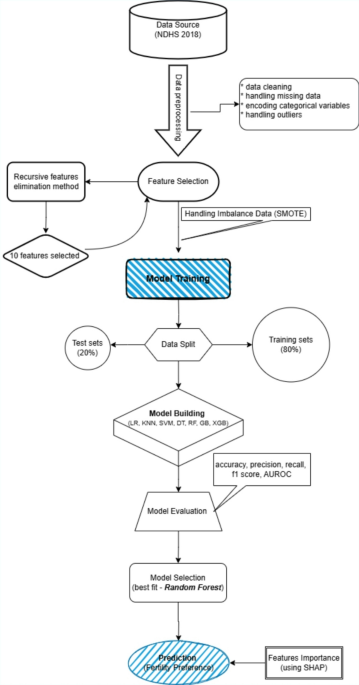
Ley, C. et al. Machine learning and conventional statistics: Making sense of the differences. Knee Surg. Sports Traumatol. Arthrosc. 30 (3), 753–757 (2022).
Rajula, H. S. R., Verlato, G., Manchia, M., Antonucci, N. & Fanos, V. Comparison of conventional statistical methods with machine learning in medicine: Diagnosis, drug development, and treatment. Medicina 56 (9), 455 (2020).
Feretzakis, G. et al. Integrating Shapley values into machine learning techniques for enhanced predictions of hospital admissions. Appl. Sci. 14 (13), 5925 (2024).
GhoshRoy, D., Alvi, P. A. & Santosh, K. C. Unboxing industry-standard ai models for male fertility prediction with SHAP. Healthcare 11 (7), 929 (2023).
GhoshRoy, D., Alvi, P. A. & Santosh, K. C. Explainable AI to predict male fertility using extreme gradient boosting algorithm with SMOTE. Electronics 12 (1), 15 (2023).
Schmeis Arroyo, V., Iosa, M., Antonucci, G. & De Bartolo, D. Predicting male infertility using artificial neural networks: A review of the literature. Healthcare 12 (7), 781 (2024).
GhoshRoy, D., Alvi, P. A. & Santosh, K. AI tools for assessing human fertility using risk factors: A state-of-the-art review. J. Med. Syst. 47 (1), 91 (2023).
GhoshRoy, D., Alvi, P. A. & Santosh, K. Leveraging sampling schemes on skewed class distribution to enhance male fertility detection with ensemble AI learners. Int. J. Pattern Recogn. Artif. Intell. 38 (02), 2451003 (2024).
Doupe, P., Faghmous, J. & Basu, S. Machine learning for health services researchers. Value Health. 22 (7), 808–815 (2019).
Ponce-Bobadilla, A. V., Schmitt, V., Maier, C. S., Mensing, S. & Stodtmann, S. Practical guide to SHAP analysis: Explaining supervised machine learning model predictions in drug development. Clin. Transl Sci. 17 (11), e70056 (2024).
Ahmed, Z. et al. Understanding the factors affecting the humanitarian health and nutrition response for women and children in Somalia since 2000: A case study. Confl. Health. 14 (1), 35 (2020).
Duale, H. A., Farah, A., Salad, A., Gele, S. & Gele, A. Constraints to maternal healthcare access among pastoral communities in the Darussalam area of Mudug region, Somalia a qualitative study. Front. Public. Health. 11, 1210401 (2023).
Wulifan, J. K., Dordah, A. D. & Sumankuuro, J. Nomadic pastoralists’ experience accessing reproductive and maternal healthcare services in low and middle-income countries: A contextual scoping review. Pastoralism 12 (1), 47 (2022).
Cronin, C. J., Guilkey, D. K. & Speizer, I. S. The effects of health facility access and quality on family planning decisions in urban Senegal. Health Econ. 27 (3), 576–591 (2018).
Yücel, U., Çiçeklioğlu, M., Öcek, Z. A. & Varol, Z. S. Access to primary health care family planning services and contraceptive use in disadvantaged women: A qualitative study. Eur. J. Contracept. Reproduct. Health Care. 25 (5), 327–333 (2020).
Adler, A., Biggs, M. A., Kaller, S., Schroeder, R. & Ralph, L. Changes in the frequency and type of barriers to reproductive health care between 2017 and 2021. JAMA Netw. Open. 6 (4), e237461–e237461 (2023).
Shatilwe, J. T., Kuupiel, D. & Mashamba-Thompson, T. P. Evidence on access to healthcare information by women of reproductive age in low-and middle-income countries: Scoping review. Plos One. 16 (6), e0251633 (2021).
Dotse-Gborgbortsi, W. et al. Distance is a big problem: A geographic analysis of reported and modelled proximity to maternal health services in Ghana. BMC Pregnancy Childbirth. 22 (1), 672 (2022).
Mseke, E. P., Jessup, B. & Barnett, T. Impact of distance and/or travel time on healthcare service access in rural and remote areas: A scoping review. J. Transp. Health. 37, 101819 (2024).
Tanou, M., Kishida, T. & Kamiya, Y. The effects of geographical accessibility to health facilities on antenatal care and delivery services utilization in benin: A cross-sectional study. Reproduct. Health. 18, 205 (2021).
Chatterjee, E. & Sennott, C. Fertility intentions and maternal health behaviour during and after pregnancy. Popul. Stud. 74 (1), 55–74 (2020).
Shumet, T. & Geda, N. R. Impacts of inequalities in utilization of key maternal health service on fertility preference among high parity women in four selected regions of Ethiopia. BMC Women’s Health. 24 (1), 590 (2024).
Dahab, R. & Sakellariou, D. Barriers to accessing maternal care in low income countries in Africa: A systematic review. Int. J. Environ. Res. Public Health. 17 (12), 4292 (2020).
Uddin, S., Khan, A., Hossain, M. E. & Moni, M. A. Comparing different supervised machine learning algorithms for disease prediction. BMC Med. Inf. Decis. Mak. 19 (1), 281 (2019).
Berger, H. & Dasré, A. Religious affiliation, education, and fertility in sub-Saharan Africa. World Dev. 184, 106723 (2024).
Bongaarts, J. Trends in fertility and fertility preferences in sub-Saharan Africa: The roles of education and family planning programs. Genus 76 (1), 32 (2020).
Idris, I. B. et al. Women’s autonomy in healthcare decision making: A systematic review. BMC Womens Health. 23, 643 (2023).
Tan, K. et al. Effects of economic uncertainty and socioeconomic status on reproductive timing: A life history approach. Curr. Res. Ecol. Soc. Psychol. 3, 100040 (2022).
Guo, C., Yang, P. & Mu, Y. Expectations of improvement of socioeconomic status throughout the life course as a component for promoting fertility intentions. China CDC Wkly. 5 (16), 365 (2023).
Matera, C. et al. Perceived economic uncertainty and fertility intentions in couples: A dyadic extension of the theory of planned behaviour. J. Fam Econ. Iss. 44 (4), 790–806 (2023).
Kigo, S. N., Omondi, E. O. & Omolo, B. O. Assessing predictive performance of supervised machine learning algorithms for a diamond pricing model. Sci. Rep. 13 (1), 17315 (2023).
Prathap, K. R. & Bhavani, R. Study comparing classification algorithms for loan approval predictability (Logistic regression, XG boost, random forest, decision Tree). J. Surv. Fisheries Sci. 10 (1S), 2438–2447 (2023).
Band, S. S. et al. Application of explainable artificial intelligence in medical health: A systematic review of interpretability methods. Inf. Med. Unlocked. 40, 101286 (2023).
Paudel, P., Saud, R., Karna, S. K. & Bhandari, M. Determining the Major Contributing Features to Predict Breast Cancer Imposing ML Algorithms with LIME and SHAP. In 2023 International Conference on Electrical, Computer and Energy Technologies (ICECET) [Internet]. IEEE; 2023 [cited 2024 Nov 23]. pp. 1–7. https://ieeexplore.ieee.org/abstract/document/10389217/
Sowjanya, A. M. & Mrudula, O. Effective treatment of imbalanced datasets in health care using modified SMOTE coupled with stacked deep learning algorithms. Appl. Nanosci. 13 (3), 1829–1840 (2023).
Kassaw, E. A., Abate, B. B., Enyew, B. M. & Sendekie, A. K. The application of machine learning approaches to classify and predict fertility rate in Ethiopia. Sci. Rep. 15 (1), 2562 (2025).
Tadese, Z. B. et al. Exploring machine learning algorithms for predicting fertility preferences among reproductive women in Nigeria. Front. Digit. Health 6:1495382 .
Barnett-Itzhaki, Z. et al. Machine learning vs. classic statistics for the prediction of IVF outcomes. J. Assist. Reprod. Genet. 37 (10), 2405–2412 (2020).
Hassan, A. A., Muse, A. H. & Chesneau, C. Machine learning study using 2020 SDHS data to determine poverty determinants in Somalia. Sci. Rep. 14 (1), 5956 (2024).
Islam, T., Meade, N., Carson, R. T., Louviere, J. J. & Wang, J. The usefulness of socio-demographic variables in predicting purchase decisions: Evidence from machine learning procedures. J. Bus. Res. 151, 324–338 (2022).
Afferri, A. et al. Policy action points and approaches to promote fertility care in the gambia: Findings from a mixed-methods study. PLOS ONE. 19 (5), e0301700 (2024).
Mohamud, L. A. & Nasir, J. A. Role of proximate determinants on the fertility rate among currently married women in Somalia via Bongaart’s model: Findings from 2018-19 Sdhs Data. 2024 [cited 2025 Jan 8]. https://www.researchsquare.com/article/rs-4752428/latest
Nyarko, S. H. Socioeconomic determinants of cumulative fertility in Ghana. Plos One. 16 (6), e0252519 (2021).
Khan, N. U. et al. Fertility patterns in pakistan: A comparative analysis of family planning trends across different geographic regions. Rural Remote Health. 24 (3), 1–8 (2024).
Lotfi, R., Rajabi Naeeni, M., Rezaei, N., Farid, M. & Tizvir, A. Desired numbers of children, fertility preferences and related factors among couples who referred to pre-marriage counseling in Alborz province, Iran. Int. J. Fertil. Steril. 11 (3), 211–219 (2017).
Weigard, A. & Spencer, R. J. Benefits and challenges of using logistic regression to assess neuropsychological performance validity: Evidence from a simulation study. Clin. Neuropsychol. 37 (1), 34 (2023).
Doepke, M., Hannusch, A., Kindermann, F. & Tertilt, M. The economics of fertility: A new era. In Handbook of the Economics of the Family [Internet]. Elsevier; 2023 [cited 2025 Jan 13]. pp. 151–254. https://www.sciencedirect.com/science/article/pii/S2949835X23000034
Jiang, Y. & Yang, F. Motherhood health penalty: Impact of fertility on physical and mental health of Chinese women of childbearing age. Front. Public. Health. 10, 787844 (2022).
Seshadri, S., Morris, G., Serhal, P. & Saab, W. Assisted conception in women of advanced maternal age. Best Pract. Res. Clin. Obstet. Gynecol. 70, 10–20 (2021).
Ahmed, J. H. J. The social context of family size decisions: The experiences of Somali and Sudanese migrant communities [Internet] [PhD Thesis]. Aston University; [cited 2025 Jan 13]. (2022). https://publications.aston.ac.uk/id/eprint/44679/
Sanogo, N. A., Fantaye, A. W. & Yaya, S. Universal health coverage and facilitation of equitable access to care in Africa. Front. Public. Health. 7, 102 (2019).
Socio-economic and demographic. factors associated with fertility preferences among women of reproductive age in Ghana: Evidence from the 2014 Demographic and Health Survey | Reproductive Health | Full Text [Internet]. 2024 [cited 2024 May 19]. https://reproductive-health-journal.biomedcentral.com/articles/https://doi.org/10.1186/s12978-020-01057-9
Ning, Y. et al. Shapley variable importance cloud for interpretable machine learning. Patterns [Internet]. 2022 [cited 2024 Dec 31];3(4). https://www.cell.com/patterns/fulltext/S2666-3899(22)00025-3
Nitsche, N. & Hayford, S. R. Preferences, partners, and parenthood: Linking early fertility desires, marriage timing, and achieved fertility. Demography 57 (6), 1975–2001 (2020).
Götmark, F. & Andersson, M. Human fertility in relation to education, economy, religion, contraception, and family planning programs. BMC Public. Health. 20 (1), 265 (2020).
Frola, A., Delprato, M. & Chudgar, A. Lack of educational access, women’s empowerment and Spatial education inequality for the Eastern and Western Africa regions. Int. J. Educ. Dev. 104, 102939 (2024).
Rajpoot, N. K., Singh, P. D., Pant, B. & Tripathi, V. The future of healthcare: A machine learning revolution. In 2023 International Conference on Artificial Intelligence for Innovations in Healthcare Industries (ICAIIHI) [Internet]. Raipur, India: IEEE; [cited 2024 Nov 23]. pp. 1–6. (2023). https://ieeexplore.ieee.org/document/10489320/
Bozkurt, S. et al. Reporting of demographic data and representativeness in machine learning models using electronic health records. J. Am. Med. Inform. Assoc. 27 (12), 1878–1884 (2020).









Leave feedback about this