The silent rhythms of sleep do more than simply restore our energy—they play a crucial role in the intricate balance of our body’s systems. Among these, blood sugar control emerges as a delicate dance influenced by the quality and quantity of our nightly rest. As the world around us buzzes with constant activity, the relationship between sleep and metabolic health often remains overlooked, yet it holds profound implications for overall well-being. This article delves into the fascinating connection between sleep patterns and blood sugar regulation, revealing how the hours we spend asleep could be just as important as the food we eat when it comes to managing our body’s vital processes.
Table of Contents
- Understanding the Connection Between Sleep and Blood Sugar Regulation
- The Impact of Sleep Deprivation on Insulin Sensitivity
- How Sleep Duration Influences Glucose Metabolism
- The Role of Sleep Quality in Managing Diabetes
- Practical Sleep Strategies to Improve Blood Sugar Control
- When to Seek Help for Sleep-Related Blood Sugar Issues
- Q&A
- Wrapping Up

Understanding the Connection Between Sleep and Blood Sugar Regulation
Sleep plays a crucial role in maintaining the body’s ability to regulate blood sugar levels effectively. When you get adequate, restful sleep, your body’s insulin sensitivity improves, allowing glucose to be absorbed more efficiently by your cells. Conversely, insufficient or poor-quality sleep disrupts the delicate hormonal balance, leading to increased insulin resistance. This means your body needs to produce more insulin to keep blood sugar levels stable, which can eventually exhaust pancreatic function and raise the risk of developing type 2 diabetes.
Key factors impacted by sleep that influence blood sugar regulation include:
- Hormone secretion: Sleep influences hormones like cortisol and growth hormone that directly affect glucose metabolism.
- Appetite regulation: Lack of sleep increases ghrelin (hunger hormone) and reduces leptin (satiety hormone), often causing overeating of sugary foods.
- Inflammation: Poor sleep increases systemic inflammation, impairing insulin signaling pathways.
| Sleep Duration | Impact on Blood Sugar |
|---|---|
| 7-9 hours | Optimal glucose regulation |
| 5-6 hours | Moderate insulin resistance |
| Less than 5 hours | Significant risk of high blood sugar |

The Impact of Sleep Deprivation on Insulin Sensitivity
Chronic lack of sleep triggers a cascade of physiological changes that diminish the body’s ability to process insulin efficiently. When we skimp on rest, the delicate balance of hormones responsible for regulating blood sugar becomes disrupted, leading to increased insulin resistance. This means glucose remains in the bloodstream longer than it should, elevating the risk for metabolic disorders. Key mechanisms include an upsurge in cortisol—the stress hormone—which antagonizes insulin’s action, coupled with diminished secretion of adiponectin, a hormone that enhances insulin sensitivity.
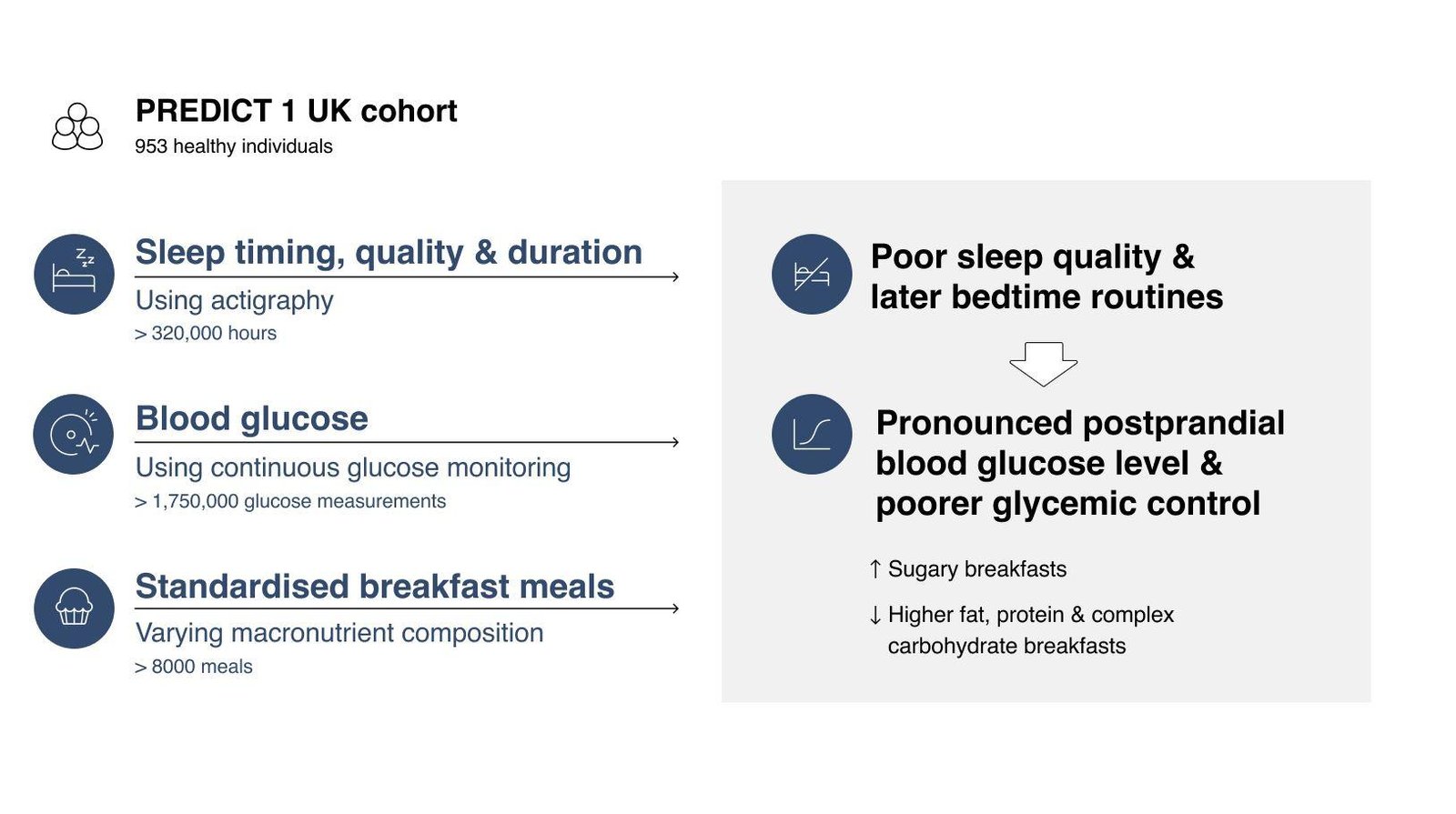
Several studies highlight the tangible effects of sleep deprivation on blood sugar control, indicating that even partial sleep loss can impair glucose metabolism. In essence, the quality and duration of sleep are as critical as diet and exercise in maintaining optimal insulin function. Consider these contributing factors to reduced insulin sensitivity linked to inadequate sleep:
- Elevated inflammatory markers that interfere with insulin signaling pathways
- Disrupted circadian rhythms altering pancreatic beta-cell function
- Increased appetite and caloric intake, often leading to weight gain
| Sleep Duration | Estimated Impact on Insulin Sensitivity |
|---|---|
| 7-9 hours | Optimal |
| 5-6 hours | Moderate Reduction |
| Less than 5 hours | Significant Reduction |
How Sleep Duration Influences Glucose Metabolism
Length of sleep plays a critical role in maintaining balanced glucose levels. Research consistently shows that both insufficient and excessive sleep can disrupt the body’s ability to regulate blood sugar, leading to impaired insulin sensitivity. During optimal sleep durations—typically 7 to 9 hours—the body’s metabolic processes effectively clear glucose from the bloodstream, supporting energy balance and reducing risks linked to diabetes.
Key mechanisms impacted by sleep duration include:
- Hormonal imbalance: Shortened sleep raises cortisol and ghrelin levels, hormones that encourage glucose production and appetite.
- Insulin resistance: Inadequate rest reduces insulin’s efficacy, making cells less responsive to glucose uptake.
- Inflammation: Poor sleep increases inflammatory markers which further impair metabolic function.
| Sleep Duration | Impact on Glucose Metabolism |
|---|---|
| Less than 6 hours | Elevated blood sugar, insulin resistance |
| 7-9 hours | Optimal glucose regulation |
| More than 10 hours | Potential metabolic disruption |

The Role of Sleep Quality in Managing Diabetes
Quality sleep is a cornerstone of effective diabetes management, influencing how your body processes insulin and regulates blood sugar levels. When sleep is fragmented or insufficient, the body’s ability to utilize insulin effectively diminishes, often leading to higher blood glucose readings. Chronic sleep deprivation can also increase stress hormones like cortisol, which further complicates blood sugar control and may push insulin resistance higher. Prioritizing restful, uninterrupted sleep can help stabilize glucose levels and support overall metabolic health.
Incorporating healthy bedtime habits can dramatically improve sleep quality and, by extension, blood sugar balance. Consider the following strategies:
- Maintain a consistent sleep schedule: Going to bed and waking up at the same times daily helps regulate your body’s internal clock.
- Create a calming bedtime environment: Reduce light exposure and loud noises to encourage deeper sleep cycles.
- Avoid stimulants: Limit caffeine and heavy meals close to bedtime, which can disrupt sleep quality.
| Sleep Duration | Impact on Blood Sugar |
|---|---|
| Less than 6 hours | Increased insulin resistance |
| 6-8 hours | Optimal glucose regulation |
| More than 9 hours | Potential risk of glucose spikes |

Practical Sleep Strategies to Improve Blood Sugar Control
Achieving stable blood sugar levels often starts with prioritizing quality sleep. One effective approach is to establish a consistent bedtime routine that signals your body it’s time to wind down. Dim lighting, screen-free time, and relaxing activities such as reading or gentle stretches can help soothe your nervous system, preparing it for restorative sleep. Incorporating a sleep schedule where you go to bed and wake up at the same time every day reinforces your circadian rhythm, which plays a vital role in glucose metabolism and insulin sensitivity.
- Create a restful environment: Use blackout curtains and a cool room temperature to optimize sleep quality.
- Limit caffeine and heavy meals: Avoid these within 4–6 hours of bedtime to prevent sleep disturbances.
- Engage in regular physical activity: Exercise improves insulin response but avoid vigorous workouts close to bedtime.
Tracking your sleep patterns alongside blood sugar readings can reveal important trends. The table below illustrates how improving sleep duration and consistency correlates with better fasting glucose levels in a hypothetical 4-week monitoring period:
| Week | Avg. Sleep Duration (hours) | Fasting Glucose (mg/dL) |
|---|---|---|
| 1 | 5.5 | 110 |
| 2 | 6.5 | 102 |
| 3 | 7.2 | 98 |
| 4 | 7.5+ | 92 |
Mindful adjustments to sleep hygiene empower you not only to rest better but also to foster a metabolic environment where blood sugar regulation thrives naturally.

When to Seek Help for Sleep-Related Blood Sugar Issues
Recognizing when to consult a healthcare professional is crucial if you experience persistent disruptions in your sleep alongside erratic blood sugar levels. If you find yourself regularly waking up with unexplained high readings, or if daytime sleepiness interferes with your ability to manage your diabetes effectively, these are red flags. Moreover, symptoms such as frequent night sweats, restless leg syndrome, or sleep apnea that coincides with fluctuating glucose levels deserve immediate attention. Ignoring these signs can worsen insulin resistance and complicate overall blood sugar control.
Consider seeking expert advice if you notice any of the following:
- Unusual fatigue despite adequate sleep
- Frequent nocturnal urination disrupting rest
- Consistent difficulty falling or staying asleep linked with glucose spikes
- Worsening glucose variability coinciding with poor sleep patterns
| Symptom | Potential Concern |
|---|---|
| Morning hyperglycemia | Dawn phenomenon or nocturnal hypoglycemia rebound |
| Excessive daytime sleepiness | Poor glucose regulation affecting energy levels |
| Loud snoring or choking during sleep | Possible sleep apnea |
| Restlessness at night | Disrupted glucose metabolism |
Q&A
Q&A:
Q1: Why does sleep influence blood sugar levels?
A1: Sleep is a vital period when your body works to regulate numerous processes, including glucose metabolism. During restful sleep, insulin sensitivity improves, allowing cells to absorb and use sugar more effectively. Poor or insufficient sleep disrupts this balance, causing higher blood sugar levels.
Q2: Can a single night of bad sleep affect my blood sugar?
A2: Yes. Even one night of inadequate or fragmented sleep can raise blood sugar levels the next day. This temporary insulin resistance can make it harder for your body to process glucose efficiently, leading to fluctuations in blood sugar.
Q3: How does chronic sleep deprivation impact those with diabetes?
A3: For people with diabetes, ongoing sleep deprivation can exacerbate blood sugar control problems. It may increase insulin resistance, making it more difficult to maintain stable glucose levels and possibly leading to more frequent episodes of hyperglycemia.
Q4: Is there a link between sleep disorders and blood sugar control?
A4: Absolutely. Conditions such as sleep apnea disrupt sleep quality and are strongly associated with impaired glucose metabolism. Treating sleep apnea can improve insulin sensitivity and overall blood sugar control.
Q5: What is the role of sleep duration and quality in managing blood sugar?
A5: Both sufficient sleep duration (typically 7–9 hours for adults) and good sleep quality are critical. Deep, uninterrupted sleep supports hormonal balance, which influences how your body manages glucose. Poor sleep quality or too little sleep can create hormonal imbalances, elevating blood sugar.
Q6: Can improving sleep habits help with blood sugar management?
A6: Yes. Establishing consistent sleep routines, creating a restful environment, and addressing sleep disorders can enhance insulin sensitivity and blood sugar regulation. Sleep hygiene is an important, often overlooked, part of managing metabolic health.
Q7: Are there specific times when sleep affects blood sugar the most?
A7: The overnight period is crucial since many metabolic processes occur during sleep, including glucose regulation. Disrupted sleep cycles or waking frequently can interrupt these processes and cause blood sugar spikes or dips during the night and into the morning.
Q8: What practical steps can I take to use sleep as a tool for better blood sugar control?
A8: Prioritize a regular sleep schedule, avoid screens before bedtime, limit caffeine and alcohol in the evening, and create a dark, cool, and quiet sleep environment. If you suspect a sleep disorder, seek professional evaluation and treatment.
Q9: How does stress during wakefulness relate to sleep and blood sugar?
A9: Stress raises cortisol levels, which can increase blood sugar. Lack of sleep amplifies stress response, creating a vicious cycle where elevated stress and poor sleep together worsen glucose metabolism.
Q10: Can naps compensate for poor nighttime sleep in controlling blood sugar?
A10: Short naps can provide some restorative benefit, but they are no substitute for consistent, quality nighttime sleep when it comes to regulating blood sugar. Relying on naps without addressing nighttime sleep issues may only offer limited metabolic benefits.
This Q&A sheds light on the critical connection between sleep and blood sugar control, emphasizing why a good night’s sleep is more than rest—it’s a metabolic regulator.
Wrapping Up
In the delicate dance of our body’s rhythms, sleep emerges not just as a nightly retreat but as a crucial partner in maintaining balanced blood sugar levels. Understanding this connection invites us to view rest not merely as a pause in activity, but as an active contributor to our metabolic harmony. As research continues to unfold, one thing remains clear: nurturing our sleep is an investment in our overall health—quietly influencing the intricate web of hormones and glucose that sustain us every day. So, as the day winds down, may we embrace rest with intention, recognizing its vital role in the ongoing symphony of blood sugar control.












Leave feedback about this