They say death is one of life’s few certainties. For a boy or young man living with Duchenne muscular dystrophy, that certainty has a cruel twist: the anticipation of dying young.
As mothers of children with this disease, we have wept helplessly in recent months as friends — fellow members of a club we never asked to join — said goodbye to their sons, the babies they once held in their arms, whose dreams they held in their hearts until Duchenne robbed them of working muscles or a healthy future.
While a Duchenne diagnosis remains absolutely terminal, it remains somehow shocking when we lose a member of our community. That is because scores of clinical trials, eight FDA-approved therapies, and a pipeline rich with additional prospects now offer this community a sense of hope and control. Progress has put a tiny asterisk on a typical Duchenne trajectory chart. The natural history of this disease is no longer predictable, and in this case, uncertainty hands-down beats the alternative.
Those therapies are now available because of risk-taking. As parents, we have each dared to enroll our children in clinical trials whose risk/benefit calculus was still being tabulated, with questions still outstanding. Each of us has had to sign lengthy consent forms acknowledging the risks of infusing our children with experimental gene therapies (one Sarepta’s, the other an earlier candidate) in these trials — risks including liver injury, acute liver failure, and death.
Still, we made the choice to sign, because our children didn’t have extra years, months, or even days to wait for help. When you’re adrift at sea, you don’t ruminate over how the rowboat might sink; you simply climb in.
Although there had been deaths associated with other AAV-mediated gene therapies for Duchenne, spinal muscular atrophy, and other conditions, Sarepta’s Elevidys had eluded that risk until recently, when the tragic deaths of two non-ambulatory patients were reported. (Separately, a patient with limb-girdle muscular dystrophy recently died after receiving a different Sarepta gene therapy.)
As with every death, the news rocked the Duchenne community, bringing shared grief for the family and a painful reminder of just how formidable our shared opponent remains. But we are experiencing another grief, too: On Friday, we learned that the FDA is asking Sarepta to stop shipment of Elevidys because of the recent deaths.
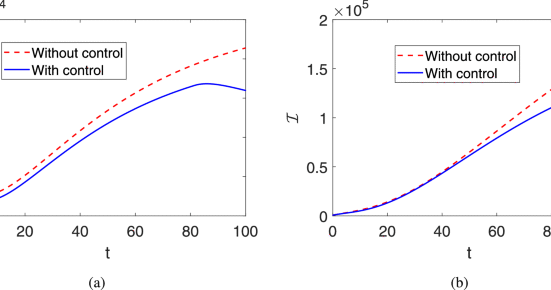
According to rules of statistics, as exposure increases, rare but known risks become statistically more observable — a classic example of the law of large numbers in pharmacovigilance. This appears to be the case for Elevidys, from which severe liver injury and failure emerged only after approximately 900 patients had been dosed through the drug’s clinical trials and commercial availability.
Of course, the loss of one life is one too many, and as human beings, we rush to understand and mitigate risk. Efforts to better characterize the conditions that led to liver failure in these cases are necessary and vital, and must be shared with physicians and families proactively, transparently, and urgently. Sarepta has announced that it has agreed to include a black box warning for Elevidys, and its convening of neuromuscular, hepatology, hematology, and immunology experts has aligned on an immunosuppressive regimen to reduce the risk of liver toxicity in non-ambulatory patients.
Yet a search for absolute safety guarantees will come up short. That luxury is not afforded to our club — and never will be.
What is guaranteed, what we are painfully reminded of every single day, is that our children are dying from their disease before our eyes. No number of risk-of-treatment warnings can mitigate the real risk of doing nothing at all. As parents, we live that reality every single day.
That’s why, without regret, we chose the risk of action over reticence. Our willingness to choose risk hinged on the FDA’s foresight to green-light trials and expedite timelines, even when questions remained and the full extent of benefits and risks would take years to understand. For diseases like Duchenne, meaningful progress demands action in the face of uncertainty. The alternative is this disease’s unchecked cruelty.
The Duchenne community has worked tirelessly to educate researchers and regulators about what it looks like to tolerate risk in rare, fatal diseases. We’ve advocated as if lives depend on it for fast-track designation, accelerated approval, and drug coverage. As a result, families have access to therapies that previous generations affected by Duchenne could only dream of.
Any moves to roll back progress, while a natural response to heartbreaking setbacks, would not bring back the patients we’ve lost to the disease or its treatment. We must avoid regressive measures that limit families’ choices, whether through regulatory restrictions or enabling insurance plans to deny our children’s right to access approved therapies. Such measures could also have a catastrophic chilling effect, creating disincentives for biotechs themselves to take on the inherent risk of innovation. Instead, we must collectively empower every step forward. Investment in science begets more options and, in turn, more science — and our children need all the science and options they can get.
New leaders at the FDA have signaled that they recognize the power of choice and access for patients and families facing diseases like Duchenne. Though we are concerned by the FDA’s recent initial rejection of Capricor’s deramiocel — Duchenne cardiomyopathy, the disease’s ultimate lethality, is an area of critical unmet need — we remain hopeful that future policies will accelerate solutions for dying patients and put decision-making in the hands of families, even when those decisions involve risk. Difficult discussions and decisions made with our doctors will always beat the alternative: no options at all.
Ultimately, in rare disease, risk is a privilege.
It is devastating when we lose lives to the hopeful pursuit of treatment, but it is equally devastating to imagine going back to a time when we had no weapons against it at all.
We must not forfeit our privilege of risk to knee-jerk wishes to remove risk from the equation entirely. Instead, families, clinicians, policymakers, and industry should work collectively to apply lessons learned from new therapies — both tragedies and triumphs — to sustain and multiply progress for the sake of patients who lack the luxury of time.
Jennifer Handt is a writer, communications adviser, and founder of Charlie’s Cure, a nonprofit that funds key research to find a cure for Duchenne muscular dystrophy. Kelly Maynard is a rare disease advocacy leader and founder of the Little Hercules Foundation, a nonprofit dedicated to unlocking treatment access for families facing rare disease. Little Hercules has received grant funding from companies working on DMD, including Sarepta.










Leave feedback about this